Original Article
Perception of “Young Adults” on Integration of Telemedicine in Healthcare Services
Licence:
Attribution-Non-commercial 4.0 International (CC BY-NC 4.0)This license enables reusers to distribute, remix, adapt, and build upon the material in any medium or format for noncommercial purposes only, and only so long as attribution is given to the creator.
Journal of Hospital Administration 9(2):p 63-70, July-December 2025. | DOI: 10.21088/jha.2582-3566.9225.2
How Cite This Article:
Tushir N, Sharma P. Perception of “young adults” on integration of telemedicine in healthcare services. RFP J Hosp Adm. 2025;9(2):63-70.Timeline
Abstract
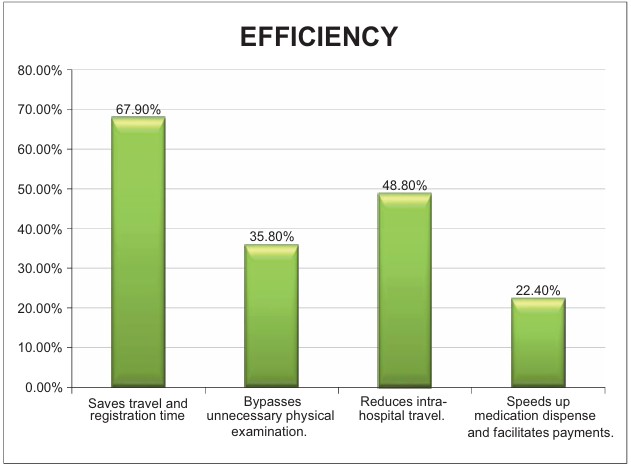
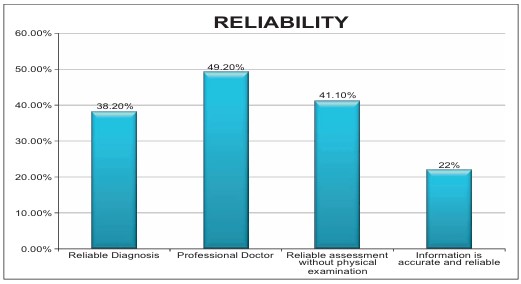
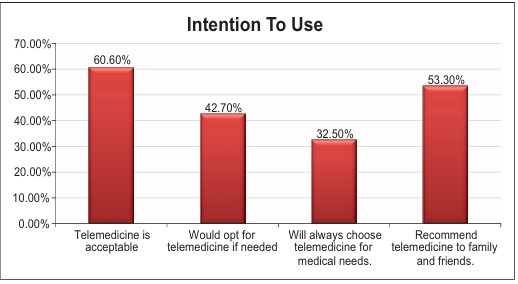
Introduction: The digital age has revolutionized healthcare delivery, with telemedicine emerging as a crucial component. The integration of telemedicine represents a paradigm shift in healthcare delivery, with young adults playing a pivotal role in shaping its adoption. Methodology: The study was conducted on 246 participants between the age range of 18 and 35 years. Data was collected using the Telemedicine Perception Questionnaire among the participants. Findings: A significant majority (63.8%) deemed telemedicine a valuable resource in healthcare. Telemedicine interaction is positively perceived, with 45.5% feeling they receive more attention, 36.6% finding communication comparable to face to-face interactions, and 56.9% expressing confidence in accessing telemedicine services when needed. Conclusion: Telemedicine offers a plethora of benefits for patients. As we continue to navigate the digital age, understanding and embracing telemedicine’s potential will be crucial in shaping the future of healthcare delivery.
References
- 1. Barney, A., Mendez-Contreras, S., Hills, N. K., Buckelew, S. M., & Raymond-Flesch, M. (2023). Telemedicine in an adolescent and young adult medicine clinic: a mixed methods study. BMC health services research, 23(1), 680.
- 2. Colucci, M., Baldo, V., Baldovin, T., & Bertoncello, C. (2019). A “matter of communication”: A to new classification compare and evaluate telehealth and telemedicine interventions and understand their effectiveness as a communication process. Health informatics journal, 25(2), 446-460.
- 3. Farhat, S. (2019). Telemedicine Adoption Across Health Care Organizations (Master›s thesis, California State University, Bakersfield)
- 4. George, A. S., & George, A. H. (2023). Telemedicine: A New Way to Provide Healthcare. Partners Universal International Innovation Journal, 1(3), 98-129.
- 5. Kehayov, I., Uchikov, P., Kitova, T., & Kitov, B. (2022). Limitations of telemedicine in low and middle-income countries. Neurosurgical Focus, 53(3), E20.
- 6. Depuru, B., Subramanyam, S. S. K., Anchapakala, S. L., & Pydipati, L. P. (2022). The Benefits and Limitations of Telemedicine During COVID-19: An Overview. Handbook of Research on Advances in Data Analytics and Complex Communication Networks, 160-167.
- 7. Guldager, R., Nordentoft, S., Bruun-Pedersen, M., & Hindhede, A. L. (2023). Social network trajectory of young adults aged 18− 35 years diagnosed with a brain tumour: a protocol for a mixed methods study. BMJ open, 13(12), e076337.
- 8. Botrugno, C. (2019). Towards an ethics for telehealth. Nursing Ethics, 26(2), 357-367.
- 9. Watson, D., Mhlaba, M., Molelekeng, G., Chauke, T. A., Simao, S. C., Jenner, S., ... & Barker, M. (2023). How do we best engage young people in decision-making about their health? A scoping review of deliberative priority setting methods. International Journal for Equity in Health, 22(1), 17.
- 10. Nyoni, T., Evers, E. C., Pérez, M., Jeffe, D. B., Fritz, S. A., Colditz, G. A., & Burnham, J. P. (2023). Perceived barriers and facilitators to the adoption of telemedicine infectious diseases consultations in Southeastern Missouri hospitals. Journal of Telemedicine and Telecare, 1357633X221149461.
- 11. Scott, R. E., & Mars, M. (2015). Telehealth in the developing world: current status and future prospects. Smart Homecare Technology and TeleHealth, 25-37.
- 12. Matsumoto, M. E., Wilske, G. C., & Tapia, R. (2021). Innovative approaches to delivering telehealth. Physical Medicine and Rehabilitation Clinics, 32(2), 451-465.
- 13. Armfield, N. R., Gray, L. C., & Smith, A. C. (2012). Clinical use of Skype: a review of the evidence base. Journal of Telemedicine and Telecare, 18(3), 125-127.
- 14. Wildevuur, S., Thomese, F., Ferguson, J., & Klink, A. (2017). Information and communication technologies to support chronic disease self management: preconditions for enhancing the partnership in person-centered care. Journal of Participatory Medicine, 9(1), e8846.
- 15. Scott Kruse, C., Karem, P., Shifflett, K., Vegi, L., Ravi, K., & Brooks, M. (2018). Evaluating barriers to adopting telemedicine worldwide: a systematic review. Journal of telemedicine and telecare, 24(1), 4-12.
- 16. Wardlow, L., Leff, B., Biese, K., Roberts, C., Archbald–Pannone, L., Ritchie, C., ... & Collaborative for Telehealth and Aging. (2023). Development of telehealth principles and guidelines for older adults: A modified Delphi approach. Journal of the American Geriatrics Society, 71(2), 371-382.
- 17. Kirubakaran, S. J., Gunasekaran, A., Dolly, D. R. J., Jagannath, D. J., & Peter, J. D. (2023). A feasible approach to smart remote health monitoring: Subscription-based model. Frontiers in public health, 11, 1150455.
- 18. Evans, Y. N., Golub, S., Sequeira, G. M., Eisenstein, E., & North, S. (2020). Using telemedicine to reach adolescents during the COVID-19 pandemic. Journal of Adolescent Health, 67(4), 469-471.
- 19. Verhoeven, F., Tanja-Dijkstra, K., Nijland, N., Eysenbach, G., & van Gemert-Pijnen, L. (2010). Asynchronous and synchronous teleconsultation for diabetes care: a systematic literature review. Journal of diabetes science and technology, 4(3), 666-684.
Data Sharing Statement
Funding
Author Contributions
Ethics Declaration
Acknowledgements
About this article
Cite this article
Tushir N, Sharma P. Perception of “young adults” on integration of telemedicine in healthcare services. RFP J Hosp Adm. 2025;9(2):63-70.
Licence:
Attribution-Non-commercial 4.0 International (CC BY-NC 4.0)This license enables reusers to distribute, remix, adapt, and build upon the material in any medium or format for noncommercial purposes only, and only so long as attribution is given to the creator.
| Received | Accepted | Published |
|---|---|---|
| September 25, 2025 | December 02, 2025 | December 24, 2025 |
DOI: 10.21088/jha.2582-3566.9225.2
Keywords
TelemedicineTelehealthHealth PerceptionHealthcare DeliverySearch for Similar Articles
Similar Articles
- Role of Fibrinogen Concentrate and Its Effect on Blood Loss in on Pump Cardiac S...
- From Sequencing to Prediction: Leveraging Next Generation Sequencing & Machine L...
- The Digital Personal Data Protection Act, 2023: Forensic and Medicolegal Implica...
- Accomplishment of International Patient Safety Goals (IPSG) in Enhancing Patient...
- Job Satisfaction and Retention Index among Nursing Officers in A Tertiary Care...
Article Level Metrics
Last UpdatedSaturday 28 February 2026, 23:24:31 (IST)
Accesses
Citations
Download citation
Article Keywords
Keyword Highlighting
Highlight selected keywords in the article text.
Timeline
| Received | September 25, 2025 |
| Accepted | December 02, 2025 |
| Published | December 24, 2025 |
licence
This license enables reusers to distribute, remix, adapt, and build upon the material in any medium or format for noncommercial purposes only, and only so long as attribution is given to the creator.