Original Article
An Occupational Hazard or Silent Burden: A Cross-sectional Exploration of Non-specific Neck Pain among Physiotherapy Practitioners
Ganu Sneha, Krishnan Vijaya, Dandekar Samiksha
Licence:
Attribution-Non-commercial 4.0 International (CC BY-NC 4.0)This license enables reusers to distribute, remix, adapt, and build upon the material in any medium or format for noncommercial purposes only, and only so long as attribution is given to the creator.
Physiotherapy and Occupational Therapy Journal 18(3):p 197-203, July-Sep 2025. | DOI: 10.21088/potj.0974.5777.18325.2
How Cite This Article:
Ganu S, Vijaya K, Samiksha D. An Occupational Hazard or Silent Burden: A Cross-sectional Exploration of Non-specific Neck Pain among Physiotherapy Practitioners. Physio Occup Ther J. 2025;18(3):197-203.Timeline
Abstract
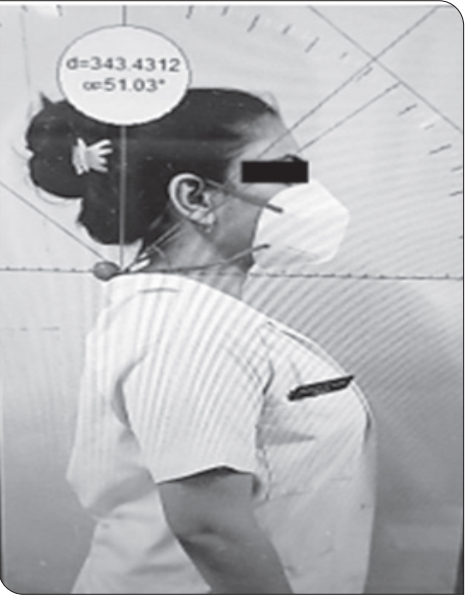
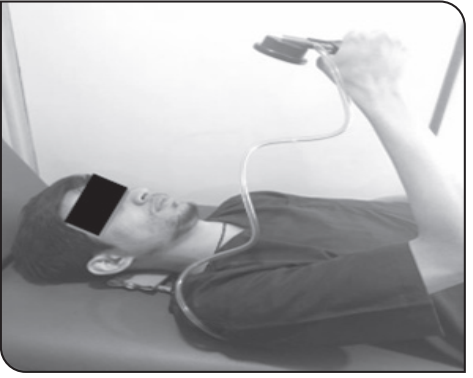
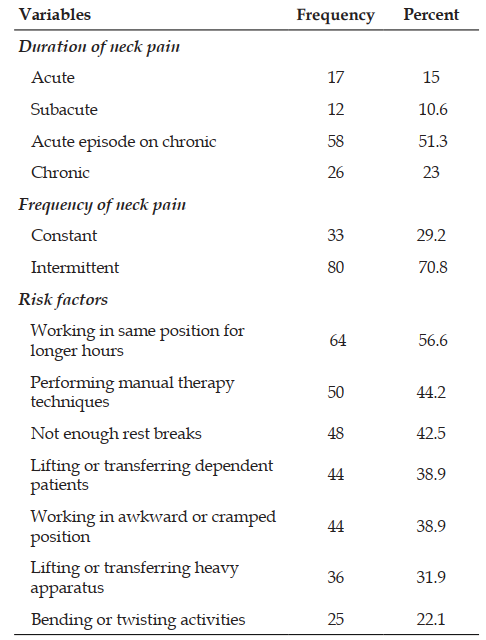
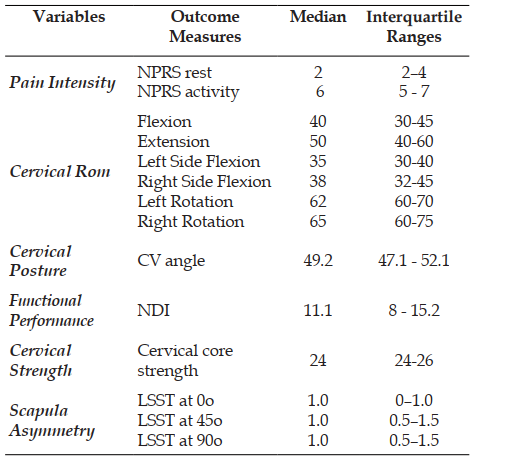
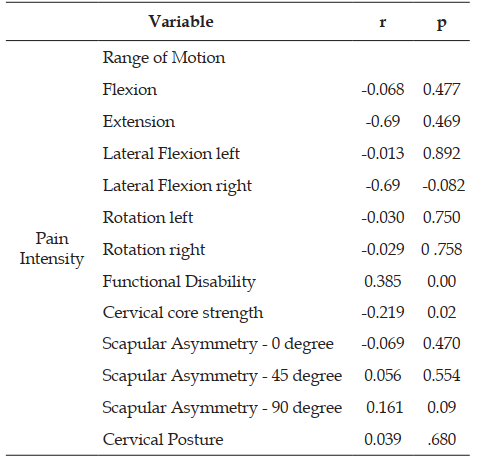
Background: Non-specific neck pain is a prevalent musculoskeletal disorder among physiotherapists, particularly associated with prolonged static postures and manual therapy techniques. Objectives: To assess non-specific neck pain and its correlation with cervical mobility, core strength, posture, functional performance, and scapular asymmetry in practicing physiotherapists. Methods: In this cross-sectional study, 113 physiotherapists (100 females, 13 males) with minimum 3 years of experience and current neck pain were recruited through purposive sampling. Assessments included cervical range of motion (universal goniometer), core strength (pressure biofeedback), craniovertebral angle (MBRuler 5.0 Software), scapular symmetry (Lateral Scapular Slide test), pain intensity (Numerical Pain Rating Scale), and functional performance (Neck Disability Index). Results: Significant correlations were found between pain intensity and functional disability (r=0.385, p<0.001), cervical core strength (r=-0.219, p=0.020), and right lateral flexion (r=-0.69, p=-0.82). Most participants (51.3%) reported acute episodes of chronic neck pain, predominantly intermittent (70.8%), with prolonged static positioning (56.6%) as the primary risk factor. Conclusions: Non-specific neck pain in physiotherapists demonstrates significant associations with reduced cervical core strength and functional performance. Pain intensity negatively correlates with cervical range of motion, particularly right lateral flexion, suggesting the need for preventive strategies and postural awareness in clinical practice.
References
- 1. Lourenço AS, Lameiras C, Silva AG. Neck flexor and extensor muscle endurance in subclinical neck pain: intrarater reliability, standard error of measurement, minimal detectable change, and comparison with asymptomatic participants in a university student population. Journal of manipulative and physiological therapeutics. 2016 Jul 1;39(6):427-33.
- 2. Guzman J, Hurwitz EL, Carroll LJ, Haldeman S, Côté P, Carragee EJ, Peloso PM, van der Velde G, Holm LW, Hogg-Johnson S, Nordin M. A new conceptual model of neck pain: linking onset, course, and care: the Bone and Joint Decade 2000–2010 Task Force on Neck Pain and Its Associated Disorders. Journal of manipulative and physiological therapeutics. 2009 Feb 1;32(2):S17-28.
- 3. Ferrari R, Russell AS. Regional musculoskeletal conditions: neck pain. Best Pract Res Clin Rheumatol. 2003 Feb;17(1):57-70.
- 4. Bovim G, Schrader H, Sand T. Neck pain in the general population. Spine (Phila Pa 1976). 1994 Jun 15;19(12):1307-9.
- 5. Hoy D, March L, Woolf A, Blyth F, Brooks P, Smith E, Vos T, Barendregt J, Blore J, Murray C, Burstein R, Buchbinder R. The global burden of neck pain: estimates from the global burden of disease 2010 study. Ann Rheum Dis. 2014 Jul;73(7):1309-15.
- 6. Cohen SP. Epidemiology, diagnosis, and treatment of neck pain. Mayo Clin Proc. 2015 Feb;90(2):284-99.
- 7. Gharote G, Piwal P, Yeole U, Adakkite R, Gawali P. Prevalence of common work related musculoskeletal pain in physiotherapy practitioners. European journal of pharmaceutical and medical research. 2016;3:398-402.
- 8. Farooq MN, Mohseni Bandpei MA, Ali M, Khan GA. Reliability of the universal goniometer for assessing active cervical range of motion in asymptomatic healthy persons. Pak J Med Sci. 2016 Mar-Apr;32(2):457-61.
- 9. Nezamuddin M, Anwer S, Khan SA, Equebal A. Efficacy of pressure-biofeedback guided deep cervical flexor training on neck pain and muscle performance in visual display terminal operators. Journal of musculoskeletal research. 2013 Sep 30;16(03):1350011.
- 10. Worlikar AN, Shah MR. Incidence of forward head posture and associated problems in desktop users. Int J Health Sci Res. 2019;9(2):96- 100.
- 11. Shadmehr A, Azarsa MH, Jalaie S. Interand intrarater reliability of modified lateral scapular slide test in healthy athletic men. Biomed Res Int. 2014;2014:384149.
- 12. Cleland JA, Childs JD, Whitman JM. Psychometric properties of the Neck Disability Index and Numeric Pain Rating Scale in patients with mechanical neck pain. Arch Phys Med Rehabil. 2008 Jan;89(1):69-74.
- 13. Hinkle DE, Wiersma W, Jurs SG. Applied statistics for the behavioral sciences. Houghton Mifflin College Division; 2003.
- 14. Lee H, Nicholson LL, Adams RD. Cervical range of motion associations with subclinical neck pain. Spine (Phila Pa 1976). 2004 Jan 1;29(1):33-40.
- 15. Kim DH, Kim CJ, Son SM. Neck Pain in Adults with Forward Head Posture: Effects of Craniovertebral Angle and Cervical Range of Motion. Osong Public Health Res Perspect. 2018 Dec;9(6):309-313.
- 16. Anderst WJ, Donaldson WF 3rd, Lee JY, Kang JD. Cervical motion segment contributions to head motion during flexion\extension, lateral bending, and axial rotation. Spine J. 2015 Dec 1;15(12):2538-43.
- 17. Ylinen J, Takala EP, Kautiainen H, Nykänen M, Häkkinen A, Pohjolainen T, Karppi SL, Airaksinen O. Association of neck pain, disability and neck pain during maximal effort with neck muscle strength and range of movement in women with chronic non-specific neck pain. Eur J Pain. 2004 Oct;8(5):473-8..
- 18. De Pauw R, Coppieters I, Kregel J, De Meulemeester K, Danneels L, Cagnie B. Does muscle morphology change in chronic neck pain patients? - A systematic review. Man Ther. 2016 Apr;22:42-9.
- 19. Schomacher J, Falla D. Function and structure of the deep cervical extensor muscles in patients with neck pain. Man Ther. 2013 Oct;18(5):360-6.
- 20. Oliveira AC, Silva AG. Neck muscle endurance and head posture: A comparison between adolescents with and without neck pain. Man Ther. 2016 Apr;22:62-7.
- 21. Akodu AK, Akinbo SR, Young QO. Correlation among smartphone addiction, craniovertebral angle, scapular dyskinesis, and selected anthropometric variables in physiotherapy undergraduates. J Taibah Univ Med Sci. 2018 Oct 5;13(6):528-534.
Data Sharing Statement
Funding
Author Contributions
Ethics Declaration
Acknowledgements
Conflicts of Interest
About this article
Cite this article
Ganu S, Vijaya K, Samiksha D. An Occupational Hazard or Silent Burden: A Cross-sectional Exploration of Non-specific Neck Pain among Physiotherapy Practitioners. Physio Occup Ther J. 2025;18(3):197-203.
Licence:
Attribution-Non-commercial 4.0 International (CC BY-NC 4.0)This license enables reusers to distribute, remix, adapt, and build upon the material in any medium or format for noncommercial purposes only, and only so long as attribution is given to the creator.
| Received | Accepted | Published |
|---|---|---|
| May 15, 2025 | June 20, 2025 | September 28, 2025 |
DOI: 10.21088/potj.0974.5777.18325.2
Keywords
Neck painPhysiotherapistsCraniovertebral AngleScapular asymmetryCross-sectional studySearch for Similar Articles
Similar Articles
- Exploring the Connection Between Stress, Anxiety, and Central Pain Mechanisms
- Comparative Effectiveness of Mulligan SNAGs and the McKenzie Method in the Mana...
- To Compare the Effectiveness of Dual Task Training Versus Task Oriented Circuit...
- Role of Virtual Reality in Physiotherapy
- Normative Values of One Leg Stance in Urban Adults of 20-40 Years
Article Level Metrics
Last UpdatedSaturday 07 February 2026, 14:23:56 (IST)
Accesses
Citations
Download citation
Article Keywords
Keyword Highlighting
Highlight selected keywords in the article text.
Timeline
| Received | May 15, 2025 |
| Accepted | June 20, 2025 |
| Published | September 28, 2025 |
licence
This license enables reusers to distribute, remix, adapt, and build upon the material in any medium or format for noncommercial purposes only, and only so long as attribution is given to the creator.