Original Article
Effectiveness of Bobath Approach Along with Core Stability Training in Stroke Patient
Niraj Kumar, Shiksha Verma, A. Patra
Licence:
Attribution-Non-commercial 4.0 International (CC BY-NC 4.0)This license enables reusers to distribute, remix, adapt, and build upon the material in any medium or format for noncommercial purposes only, and only so long as attribution is given to the creator.
Physiotherapy and Occupational Therapy Journal 16(2):p 85-96, April–June 2023. | DOI: http://dx.doi.org/10.21088/potj.0974.5777.16223.3
How Cite This Article:
Verma S, Kumar N, Patra A. Effectiveness of Bobath approach along with core stability training in stroke patient. Physiother Occup Ther J. 2023;16(2):85-96.Timeline
Abstract
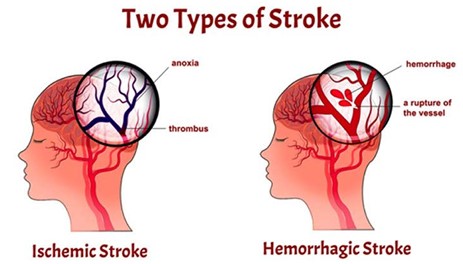
Introduction: Physiologically stroke is an acute, focal injury of the central nervous system of a vascular origin, contributing to a local or systemic neurological insult. Stroke one side of the upper and lower limbs are affected but trunk muscle are affected on both sides leading to insufficient trunk rotation and difficulty in maintain balance. Restoration of trunk control and balance is one of the important goals in rehabilitation of stroke patients. Neuro developmental therapy (NDT) is one of the preferred methods of stroke rehabilitation, also known as bobath concept. With the fine control and proper weight transfer, it is possible to secure and protect the body in upright posture and in the achievement distal functional movements. Purpose of Study: In comparison to limb muscles weakness, trunk muscle are also impaired in both ipsilateral and contralateral side of the body, thus weakness of the trunk muscle leads to loss of balance, stability and increase functional disability. This limits the patient’s activities, such as rolling in bed, transferring, putting on a shirt and bending to reach his feet to put on shoes and socks, etc. So my aim is to focus on the trunk function and balance in stroke patient in order to eliminate individual trunk impairment affecting various functions performed by the patients. Hence the purpose of the study to evaluate the effectiveness of the stroke patient. Methodology: Total 15 patients were included in the study by simple random sampling method. Group A (Experimental group) was received bobath approach and core stability training exercises. Conclusion: Bobath approach along with core stability training shows more improvement in trunk function and sitting balance after 4 week therapy.
References
- 1. Hye-Jin Lee, Tae-Woo Kang, et al. (2018). Effects of diaphragm and deep abdominal muscle exercise on walking and balance ability in patients with hemiplegia due to stroke. Journal of exercise rehabilitation 2018, volume 14 (4): page no. 648-653; doi.org/10.12965/ jer.1836252.
- 2. Puthenpurakala and Crussel J (2017) Stroke 1: definition, burden, riskfactors and diagnosis. Nursing time, vol.113, pp43-47.
- 3. Fujita T, Sato A, et al. (2015). Contribution of abdominal muscle strength to various activities of daily living of stroke patients with mild paralysis. J PhysTHer Sci. 2015;27(3):815-818. Doi:10.1589/jpts.27.815.
- 4. Horak FB. postural orientation and equilibrium: what do we need to know about neutral control of balance to prevent falls? Age Ageing.2006;35:ii7ii11:doi:10.1093/ageing/afl077.
- 5. Evelyne Wiskerke et al. maximum weight shifts in non-ambulatory people with stroke are related to trunk control and balance: a cross sectional study. Epub 2020; 83:121-126. Doi10.1016/j.gaitpost.2020.10.007.
- 6. Vishal Sharma, Jaskirat Kaur (2017). Effect of core strengthening with pelvic proprioceptive neuromuscular facilitation on trunk, balance, gait and function in chronic stroke. Journal of exercise rehabilitation 2017;13(2):200-205; doi:10.12965/jer.1734892.446.
- 7. Mudie m, Winzeler-Mercay, et al. training symmetry of weight distribution after stroke: a randomized controlled pilot study comparing task related reach. Bobath and feedback training approaches. Clin Rehab. 2002;16(6):582-592. Doi:10.1191/0269215502cr527oa.
- 8. Panel, J.P.Mohar, Gregory W et al. 2017. Etiology of stroke. Stroke; vol.28(7):pp1501-06.
- 9. Xibo Sun, MD, Qian Gao et al. 2016. Which is better in the rehabilitation of stroke patients, core stability exercises or conventional exercises? The journal of physical sciences. vol:28;pp:1131-1133; doi:10.1589/jpts.28.1131.
- 10. Niraj Kumar1, Navneet Badoni2, Siddhartha Sen3, AnirbanPatra 4, Shobit Garg5 Kanchan Joshi 6 (2022), Effectiveness of Mindfulness Based Stress Reduction Therapy (MBSRT) on Anxiety and depression, Quality of Life and Mindfulness in Diabetic Frozen Shoulder Conditions, Journal of Positive School Psychology, Volume-6, Issue-2, Pages 2291 – 2308, http://journalppw.com.
- 11. Pablo M Lavados, et al. (2021). Incidence, risk factors, prognosis, and health-related quality of life after stroke in a low-resource community in chile (NANDU): a prospective population- based study, volume 9, issue 3, E340-351, march01, 2021;doi:10.1016/S22140 109X(20)30470-8.
- 12. Yu SH, Park SD: The effects of core stability strength exercise on muscle activity and trunk impairment scale in stroke patients. J Exer Rehabil, 2013, 9: 362-367.
- 13. AyukoKaji, Shun Sasagawa, et al. (2010). Transient effect of core stability exercises on postural sway during quiet standing. Journal of strength and conditioning research;vol:24(2);pp:382-388;doi: JSC.0b013e3181c06bdd. 10.1519/
- 14. Shizuka Sasaki, Eiichi Tsuda, et al. (2019). Core muscle training and neuromuscular control of the lower limb and trunk. Journal of athletics training; 2019;54(9):959-969; doi:10.4085/1062 6050-113-17.
- 15. Barnes MP. An overview of the clinical management of spasticity. In: upper motor neuron syndrome and spasticity: clinical management and neurophysiology. Eds: Barnes MP, Johnson GTR. Cambridge University Press 2001.
- 16. Julie Vaughan Graham, Catherine Eustace, et al. The bobath concept in contemporary clinical practice. Top stroke Rehabil 2009;16(1):57-68; doi: 10.1310/trs1601-57.
- 17. Alwin Puthenpurakal, et al. Stroke 1: definition, burden, risk factors and diagnosis.2011vol 113 issue 11.
- 18. Jyotisharma, Niraj Kumar, Shashank Kumar. Comparison of the effectiveness of core strengthening exercise and Mckenzie exercise on the pain functional disability in lumbar PIVD condition. Physiotherapy and occupational therapy Journal Volume 11 Number2, April- June 2018 DOI: http://dx.doi.org/10.21088/ potj.0974.5777.11218.4.
- 19. Raine S. Defining the Bobath concept using the Delphi technique. Physio Res Int. 2006; 11:4-13.
- 20. V. S. Caviness, Dphil N. Makris, (2002) et al. Anatomy of stroke part I, Stroke; vol.33: pp2549-56.
- 21. Ethan A. Prince and Sun Ho Ahn, (2013) Basic Vascular Neuroanatomy of the Brain and Spine: What the General Interventional Radiologist Needs to Know, SeminInterventRadiol; vol.30: pp234–239.
- 22. B. D Chaurasia’s, Human anatomy vol.3, 6th edition; pp455-61.
- 23. Tamaya Van Criekinge, Steven Truijen, et al. The effectiveness of trunk training on trunk control, sitting and standing balance and mobility post-stroke: a systematic review and meta-analysis. Sagepub.com/journals permissions. DOI: 10.1177/0269215519830159.
- 24. Chen X, Gan Z, Tian W, Lv Y. effect of rehabilitation training of core muscle stability on stroke patient with hemiplegia. Pak J Med SCI. 2020;36(3): 461-466. DOI: https://doi. org/10.12669/pjms.36.3.1466.
- 25. G Varadharajulu, Lathika Shetty, Kulamani Sahoo. The effect of bobath concept and conventional approach on the, functional outcome in the Post stroke Hemiplegic Individuals. IOSR Journal of sports and Physical Education (IOSR-JSPE) e-ISSN: 2347 6737, p-ISSN: 2347-6745, Volume 4, Issue 2, (Mar.-Apr.), PP10-14.
- 26. Seung- heon (2017) et al. The effect of trunk exercise on mobility, balance and trunk control of stroke patients. J Korean SocPhys Med, 2017; 12(1) : 25-27.doi:10.13066/kspm.2017.12.1.25.
- 27. Julee Das, R. Raja, R. Vedavathi. A Study to Assess the Effectiveness of Trunk Rehabilitation Programme on Trunk Control And Balance in Acute Ischemic Hemiparetic Stroke Patients. IOSR Journal of Dental and Medical Sciences (IOSR-JDMS) e-ISSN: 2279-0853, p-ISSN: 2279-0861. Volume15, Issue12. Ver. VIII (December.2016), PP72-8.
- 28. Muhammed KilinicAvcu, et al. (2016). The effects of Bobath-based trunk exercises on trunk control, functional capacity, balance, and gait: a pilot randomized controlled trail, topics in stroke rehabilitation, 23:1, 50-58, DOI:10.117 9/1945511915Y.0000000011.
- 29. Raikan Buyukavec, Fusum Sahin (Oct 2015) et al. The impact of additional trunk balance exercises on balance, functional condition and ambulation in early stroke patients. Turk J Phys Med Rehab 2016;62(3):248-256; doi: 10.5606/ tftrd.2016.84770.
- 30. Rosa Cabanas-Valdes, Caritat Bagur-Calafat, et al. The effect of core stability exercises on improving dynamic sitting balance and trunk control for sub-acute stroke patient: A randomized controlled trial. Sagepub.co.uk/journals Permission.nav;D OI:10.1177/0269215515609414.
- 31. Hanan Helmy, Tamer Emara (July 2014) et al. Impact of of trunk control on balance and functional abilities in chronic stroke patients. Egypt J Neurol Psychiat Neurosurg.; july 2014;vol:5;issue 3.
- 32. Niraj Kumar, Siddhartha Sen, Navneet Badoni Anirban Patra Sobhit Garg (2022) International Journal of Health Sciences, Volume-6, Issue, S1, Pages-2630–2645.https://doi.org/10.53730/ ijhs.v6nS1.5338.
- 33. Seong-Hun yu (June 2013) et al. The effect of core stability strength exercise on muscle activity and trunk impairment scale in stroke patients. J exercRehabil. 2013 jun;9(3):362-367; doi: 10.12965/jer.130042.
- 34. SudhaDhami, Niraj Kumar, Niranjan Kumar et al. (2019) Mirror Therapy and Repetitive Facilitation Exercise Improve the Upper Extremity Motor Recovery in Hemiparesis Patients, Physiotherapy and Occupational Therapy Journal, Volume 12 Number 1, PP- 58-67 DOI:http://dx.doi.org/10.21088/ potj.0974.5777.12119.8.
- 35. Niraj Kumar, Navneet Badoni2, Siddhartha Sen et. al. (2022) Effectiveness of Mindfulness Based Stress Reduction Therapy (MBSRT) on Anxiety and depression, Quality of Life and Mindfulness in Diabetic Frozen Shoulder Conditions. Vol. 6, No. 2, PP-2291 – 2308 http://journalppw.com.
Data Sharing Statement
Funding
Author Contributions
Ethics Declaration
Acknowledgements
Conflicts of Interest
About this article
Cite this article
Verma S, Kumar N, Patra A. Effectiveness of Bobath approach along with core stability training in stroke patient. Physiother Occup Ther J. 2023;16(2):85-96.
Licence:
Attribution-Non-commercial 4.0 International (CC BY-NC 4.0)This license enables reusers to distribute, remix, adapt, and build upon the material in any medium or format for noncommercial purposes only, and only so long as attribution is given to the creator.
| Received | Accepted | Published |
|---|---|---|
| May 13, 2023 | June 05, 2023 | June 29, 2023 |
DOI: http://dx.doi.org/10.21088/potj.0974.5777.16223.3
Keywords
Stroke; Bobath Approach; TIS; BBS; Core Stability.StrokeBobath ApproachTISBBSCore StabilitySearch for Similar Articles
Similar Articles
- Exploring the Connection Between Stress, Anxiety, and Central Pain Mechanisms
- Comparative Effectiveness of Mulligan SNAGs and the McKenzie Method in the Mana...
- To Compare the Effectiveness of Dual Task Training Versus Task Oriented Circuit...
- Role of Virtual Reality in Physiotherapy
- Normative Values of One Leg Stance in Urban Adults of 20-40 Years
Article Level Metrics
Last UpdatedSaturday 07 February 2026, 14:21:40 (IST)
Accesses
Citations
Download citation
Article Keywords
Keyword Highlighting
Highlight selected keywords in the article text.
Timeline
| Received | May 13, 2023 |
| Accepted | June 05, 2023 |
| Published | June 29, 2023 |
licence
This license enables reusers to distribute, remix, adapt, and build upon the material in any medium or format for noncommercial purposes only, and only so long as attribution is given to the creator.