Review Article
Recent Advance in Transdermal Patch
Sandhiya , N Deepa, Salma R, Rajavignesh S, Santhanalakshmi K, Shanmuga Sundaram S, Sharon Mahim
Licence:
Attribution-Non-commercial 4.0 International (CC BY-NC 4.0)This license enables reusers to distribute, remix, adapt, and build upon the material in any medium or format for noncommercial purposes only, and only so long as attribution is given to the creator
RFP Journal of Dermatology 9(1):p 25-29, January–June 2024. | DOI: NA
How Cite This Article:
Sandhiya, Deepa N, Salma R, et al. Recent Advance in Transdermal Patch. RFP Jr of Drea. 2024;9(1):25-29.Timeline
Abstract
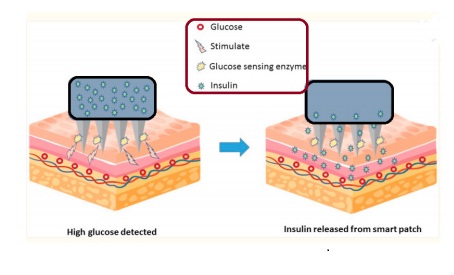
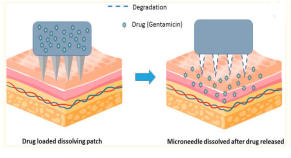
Drug administration with transdermal patches is a non-invasive technique. It is an adhesive patch that is intended to penetrate the skin and enter the bloodstream, distributing a precise dosage of medication throughout the body. Compared to other administration methods, transdermal medication delivery is less intrusive, more patient-friendly, and able to avoid first-pass metabolism and the harmful acidic environment of the stomach that arises from oral drug absorption. Transdermal patches have garnered interest and been used for many years to treat a variety of illnesses and ailments. These medications include nitroglycerin, clonidine, nicotine, and fentanyl. This approach has also been investigated recently for the delivery of biologics in several applications. Here, we examine the body of research on the design
References
- 1. Dull P. Transdermal oxybutynin (oxytrol) for urinary incontinence. Am. Fam. Physician. 2004;70:2351–2352.
- 2. Ho C. Transdermally-delivered oxybutynin (Oxytrol(R) for overactive bladder. Issues Emerg. Health Technol. 2001;24:1–4.
- 3. KurzA.,FarlowM.,LefevreG.Pharmacokinetics of a novel transdermal rivastigmine patch for the treatment of Alzheimer’s disease: A review. Int. J. Clin. Pract. 2009;63:799–805. doi: 10.1111/j.1742-1241.2009.02052.x.
- 4. Lefevre G., Pommier F., Sedek G., Allison M., Huang H.L., Kiese B., Ho Y.Y., Appel-Dingemanse S. Pharmacokinetics and bioavailability of the novel rivastigmine transdermal patch versus rivastigmine oral solution in healthy elderly subjects. J. Clin. Pharmacol. 2008;48:246–252. doi: 10.1177/0091270007312154.
- 5. (Neupro) for the treatment of Parkinson’s disease. Issues Emerg. Health Technol. 2008;112:1–6.
- 6. Jessen L., Kovalick L.J., Azzaro A.J. The selegiline transdermal system (emsam): A therapeutic option for the treatment of major depressive disorder. P T Peer-Rev. J. Formul. Manag. 2008;33:212–246.
- 7. Johnson P., Hansen D., Matarazzo D., Petterson L., Swisher C., Trappolini A. Transderm Scop for prevention of motion sickness. N. Engl. J. Med. 1984;311:468–469. doi: 10.1056/ NEJM198408163110713.
- 8. Swaminathan S.K., Strasinger C., Kelchen M., Carr J., Ye W., Wokovich A., Ghosh P., Rajagopal S., Ueda K., Fisher J., et al. Determination of Rate and Extent of Scopolamine Release from Transderm Scop(R) Transdermal Drug Delivery Systems in Healthy Human Adults. AAPS PharmSciTech. 2020;21:117. doi: 10.1208/ s12249-020-01658-4.
- 9. Bhasin S., Storer T.W., Asbel-Sethi N., Kilbourne A., Hays R., Sinha-Hikim I., Shen R., Arver S., Beall G. Effects of testosterone replacement with a nongenital, transdermal system, Androderm, in human immunodeÀciency virus-infected men with low testosterone levels. J. Clin. Endocrinol. Metab. 1998;83:3155–3162. doi: 10.1210/jc.83.9.3155.
- 10. De Sanctis V., Vullo C., Urso L., Rigolin F., Cavallini A., Caramelli K., Daugherty C., Mazer N. Clinical experience using the Androderm testosterone transdermal system in hypogonadal adolescents and young men with beta-thalassemia major. J. Pediatr. Endocrinol. Metab. 1998;11((Suppl. 3)):891–900.
- 11. Buch A., Shen L., Kelly S., Sahota R., Brezovic C., Bixler C., Powell J. Steady-state bioavailability of estradiol from two matrix transdermal delivery systems, Alora and Climara. Menopause. 1998;5:107–112. doi: 10.1097/00042192-199805020-00009.
- 12. Rozenbaum H., Birkhauser M., De Nooyer C., R., Pornel B., Schneider H., Studd J. Comparison of two estradiol transdermal systems (Oesclim 50 and Estraderm TTS 50). I. Tolerability, adhesion and efÀcacy. Maturitas. 1996;25:161– 173. doi: 10.1016/S0378-5122(96)01068-7.
- 13. Youngkin E.Q. Estrogen replacement therapy and the estraderm transdermal system. Nurse Pract. 1990;15:19–26, 31. doi: 10.1097/00006205- 199005000-00005.
- 14. Wokovich A.M., Prodduturi S., Doub W.H., Hussain A.S., Buhse L.F. Transdermal drug delivery system (TDDS) adhesion as a critical safety, efÀcacy and quality attribute. Eur. J. Pharm. Biopharm. 2006;64:1–8. doi: 10.1016/j. ejpb.2006.03.009.
- 15. Kim Y.C., Park J.H., Prausnitz M.R. Microneedles for drug and vaccine delivery. Adv. Drug Deliv. Rev. 2012;64:1547–1568. doi: 10.1016/j.addr.2012.04.005.
- 16. Li W.Z., Huo M.R., Zhou J.P., Zhou Y.Q., Hao B.H., Liu T., Zhang Y. Super-short solid silicon microneedles for transdermal drug delivery applications. Int. J. Pharm. 2010;389:122–129. doi: 10.1016/j.ijpharm.2010.01.024.
- 17. Permana A.D., Tekko I.A., McCrudden M.T.C., Anjani Q.K., Ramadon D., McCarthy H.O., Donnelly R.F. Solid lipid nanoparticlebased dissolving microneedles: A promising intradermal lymph targeting drug delivery system with potential for enhanced treatment of lymphatic Àlariasis. J. Control. Release. 2019;316:34–52. doi: 10.1016/j. jconrel.2019.10.004.
- 18. Cheung K., Das D.B. Microneedles for drug delivery: Trends and progress. Drug Deliv. 2016;23:2338–2354. doi: 10.3109/10717544.2014.986309.
- 19. Ita K. Transdermal Delivery of Drugs with Microneedles-Potential and Challenges. Pharmaceutics. 2015;7:90–105. doi: 10.3390/ pharmaceutics7030090.
- 20. Ashraf M.W., Tayyaba S., Nisar A., Afzulpurkar N., Bodhale D.W., Lomas T., Poyai A., Tuantranont A. Design, fabrication and analysis of silicon hollow microneedles for transdermal drug delivery system for treatment of hemodynamic dysfunctions. Cardiovasc. Eng. 2010;10:91–108. doi: 10.1007/s10558-010-9100-5.
- 21. O’Mahony C., Sebastian R., Tjulkins F., Whelan D., Bocchino A., Hu Y., O’Brien J., Scully J., Hegarty M., Blake A., et al. Hollow silicon microneedles, fabricated using combined wet and dry etching techniques, for transdermal delivery and diagnostics. Int. J. Pharm. 2023;637:122888. doi: 10.1016/j. ijpharm.2023.122888.
- 22. Ma Y., Gill H.S. Coating solid dispersions on microneedles via a molten dip-coating method: Development and in vitro evaluation for transdermal delivery of a water-insoluble drug. J. Pharm. Sci. 2014;103:3621–3630. doi: 10.1002/ jps.24159.
- 23. B.Z., He M.C., Zhang X.P., Fei W.M., Cui Y., Guo X.D. A novel method for fabrication of coated microneedles with homogeneous and controllable drug dosage for transdermal drug delivery. Drug Deliv. Transl. Res. 2022;12:2730– 2739. doi: 10.1007/s13346-022-01123-8.
- 24. Chen Y., Chen B.Z., Wang Q.L., Jin X., Guo X.D. Fabrication of coated polymer microneedles for transdermal drug delivery. J. Control. Release. 2017;265:14–21. doi: 10.1016/j. jconrel.2017.03.383.
- 25. Gill H.S., Prausnitz M.R. Coated microneedles for transdermal delivery. J. Control. Release. 2007;117:227–237. doi: 10.1016/j. jconrel.2006.10.017.
- 26. Dalvi M., Kharat P., Thakor P., Bhavana V., Singh S.B., Mehra N.K. Panorama of dissolving microneedles for transdermal drug delivery. Life Sci. 2021;284:119877. doi: 10.1016/j. lfs.2021.119877.
- 27. Dillon C., Hughes H., O’Reilly N.J., McLoughlin P. Formulation and characterisation of dissolving microneedles for the transdermal delivery of therapeutic peptides. Int. J. Pharm. 2017;526:125–136. doi: 10.1016/j.ijpharm.2017.
Data Sharing Statement
Funding
Author Contributions
Ethics Declaration
Acknowledgements
Conflicts of Interest
About this article
Cite this article
Sandhiya, Deepa N, Salma R, et al. Recent Advance in Transdermal Patch. RFP Jr of Drea. 2024;9(1):25-29.
Licence:
Attribution-Non-commercial 4.0 International (CC BY-NC 4.0)This license enables reusers to distribute, remix, adapt, and build upon the material in any medium or format for noncommercial purposes only, and only so long as attribution is given to the creator
| Received | Accepted | Published |
|---|---|---|
| March 28, 2024 | April 23, 2024 | June 30, 2024 |
DOI: NA
Keywords
Transdermal patchTypesAdvance in transdermal patchSearch for Similar Articles
Similar Articles
- Delving into Wolf’s Isotopic Phenomenon: Tale of Two Cases of Psoriasis Localize...
- Pachydermoperiostosis, Complete Form: A Case Report of Rare Occurrence
- Role of Cyclical Negative Pressure Wound Therapy in Thermal Burns
- Annular Keloid Mimicking Granuloma Annulare: A Diagnostic Challenge
- Dermatological Care for All: A Perspective
Article Level Metrics
Last UpdatedMonday 26 January 2026, 18:54:47 (IST)
Accesses
Citations
Download citation
Article Keywords
Keyword Highlighting
Highlight selected keywords in the article text.
Timeline
| Received | March 28, 2024 |
| Accepted | April 23, 2024 |
| Published | June 30, 2024 |
licence
This license enables reusers to distribute, remix, adapt, and build upon the material in any medium or format for noncommercial purposes only, and only so long as attribution is given to the creator