Original Article
Obstructive Sleep Apnea (OSA) and its Association with Depression
Md Adil Faizan, , Md Adil Faizan1 , K Sri Divya Reddy2 , Geethanjali3 , M Raghuram4 , R Sateesh Babu5
Licence:
RFP Indian Journal of Medical Psychiatry 7(2):p 43-47, July - Dec 2024. | DOI: n.a
How Cite This Article:
Md Adil Faizan, K Sri Divya Reddy, et al., Obstructive Sleep Apnea (OSA) and its Association with Depression. RFP Ind Jr of Med Psy. 2024;7(2):43–47
Timeline
Abstract
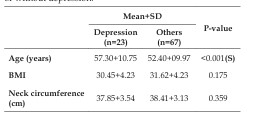
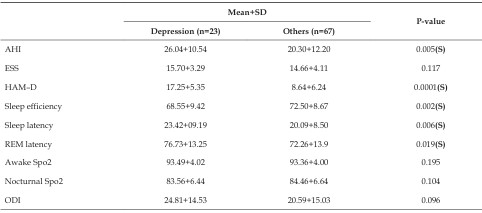
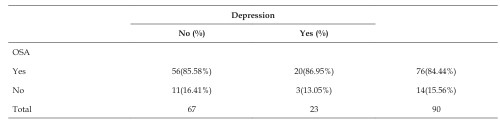
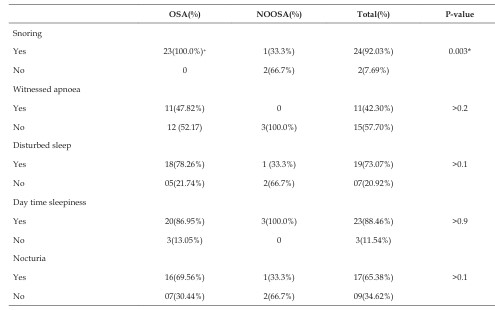
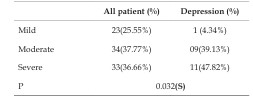
Objective: This study investigates the correlation between Obstructive Sleep Apnea (OSA) and depression, examining how OSA impacts psychiatric well-being and quality of life. Introduction: Obstructive Sleep Apnea (OSA) is characterized by episodes of partial or complete airway obstruction during sleep, leading to fragmented and non-restorative sleep. OSA has significant implications for mental health, including a strong association with depression and other psychiatric conditions. Despite considerable evidence linking OSA with psychiatric symptoms, the precise nature of this relationship remains ambiguous. Methods: A cross-sectional study was conducted with 182 participants at a tertiary care center in Telangana from July 2022 to June 2023. Tools employed included the Epworth Sleepiness Scale (ESS), Polysomnography (PSG), and the Hamilton Depression Rating Scale (HAM-D). Participants included those referred for PSG who consented to the study. Exclusions were made for patients with nocturnal oxygen supplementation, recent upper airway surgery, or unstable cardiopulmonary, neurological, or psychiatric conditions. Results: Out of 90 patients who underwent PSG, 23 were diagnosed with depression. These patients were significantly older (mean age 57.30 years) compared to non-depressed individuals (mean age 52.40 years, P < 0.001). Depression was associated with higher HAM-D scores (mean 17.25) and poorer sleep efficiency (68.55%) compared to non-depressed patients (HAM-D mean 8.64, sleep efficiency 72.50%). Additionally, depressed patients exhibited longer sleep latency and REM latency. The Apnoea-Hypopnoea Index (AHI) was significantly higher in depressed patients (mean 26.04) compared to non-depressed patients (mean 20.30, P = 0.005). The majority of depressed patients had abnormal PSG results, with 91.3% showing aberrant findings. Discussion: The study confirms a significant association between OSA and depression. Depression exacerbates OSA symptoms and impairs sleep quality, with substantial implications for patient management and treatment outcomes. The link between OSA and psychiatric conditions such as depression highlights the need for integrated treatment approaches that address both sleep and mental health issues. Conclusion: OSA is prevalent among individuals with depression, and its impact on psychiatric well-being is considerable. Clinicians should be vigilant in screening for OSA in depressed patients to improve overall treatment outcomes. Further research is needed to explore the mechanisms underlying the OSA-depression connection and to develop comprehensive management strategies.
References
No records found.
Data Sharing Statement
Funding
Author Contributions
Ethics Declaration
Acknowledgements
Conflicts of Interest
About this article
Cite this article
Md Adil Faizan, K Sri Divya Reddy, et al., Obstructive Sleep Apnea (OSA) and its Association with Depression. RFP Ind Jr of Med Psy. 2024;7(2):43–47
Licence:
| Received | Accepted | Published |
|---|---|---|
| N/A | N/A | N/A |
DOI: n.a
Keywords
Obstructive Sleep ApneaDepressionPolysomnographyPsychiatric ComorbiditySleep Disorders.Article Level Metrics
Last UpdatedMonday 26 January 2026, 19:17:03 (IST)
Accesses
Citations
Download citation
Article Keywords
Keyword Highlighting
Highlight selected keywords in the article text.
Timeline
| Received | N/A |
| Accepted | N/A |
| Published | N/A |