Original Article
Effect of Physiotherapy Intervention in Temporomandibular Joint Dysfunction
Akshay Pal, Anand Misra, Piyush Jain, Jitendra Sharma
Licence:
Attribution-Non-commercial 4.0 International (CC BY-NC 4.0)This license enables reusers to distribute, remix, adapt, and build upon the material in any medium or format for noncommercial purposes only, and only so long as attribution is given to the creator.
Physiotherapy and Occupational Therapy Journal 17(3):p 133-139, July-September 2024. | DOI: http://dx.doi.org/10.21088/potj.0974.5777.17324.1
How Cite This Article:
Misra A, Pal A, Jain P, et al. Effect of physiotherapy intervention in temporomandibular joint dysfunction. Physio Ther Occup Ther J. 2024;17(3):133-139.Timeline
Abstract
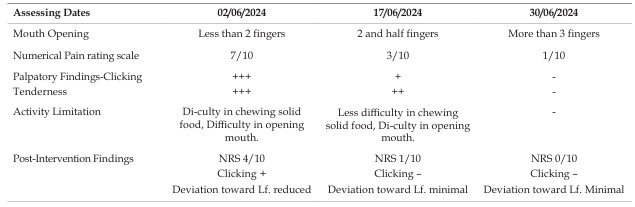
condition of the human body. Temporomandibular joint (TMJ) dysfunction is a challenging and often unbearable condition characterized by pain in the joint and surrounding muscles, often resulting in stiffness, complications, earache, malocclusion, clicking sounds, and trismus. TMJ dysfunction is frequently linked to imbalances in the body, particularly in the neck and shoulders. Misdiagnosis or inadequate management can lead to chronic pain syndromes, which can be distressing for patients. This condition may present as acute or chronic; while acute TMJ dysfunction is commonly managed with manual reduction, chronic cases are more complex. Case Description: We report the case of an 18-year-old male athlete referred by his dentist for conservative management of TMJ dysfunction. He presented with left jaw pain for the past four months, limited mouth opening, jaw clicking, and difficulty chewing hard foods, accompanied by tenderness in the neck, mouth, and cheek muscles. We assessed, diagnosed, and proposed treatment options for this patient. Management & Outcomes: The patient’s TMJ dysfunction was managed conservatively through physical therapy as the first line of treatment. By the end of the intervention, he reported being pain-free and had regained normal TMJ function. This case highlights the role of physiotherapy in managing TMJ disorders. Although various treatments exist, evidence for their efficacy in TMD remains limited, and no standard protocol is established. Common treatment options include occlusal splints, cognitive behavioral therapy, and pain medications. Result: Non-invasive physiotherapy treatments have proven effective in alleviating symptoms of TMJ dysfunction. The initial focus is on pain relief and muscle spasm reduction, employing techniques such as pulsed ultrasound and manual therapy, including dry needling to address trigger points. Discussion: TMJ dysfunction may be associated with overall body imbalances, as increased muscle tension in the upper body can lead to compensatory adjustments affecting spinal muscle tension. A conservative management strategy centered on physical therapy is recommended. Physical therapists are well-positioned to provide clinical support for TMD patients, creating rehabilitation plans tailored to each individual’s impairments. Conclusion: This case report suggests that a conservative management approach, incorporating pain management strategies, muscle strengthening, and the release of trigger points and tight muscles, may significantly benefit individuals suffering from TMJ dysfunction.
References
- 1. Lomas J, Gurgenci T, Jackson C, Campbell D. Temporomandibular dysfunction. Aust J Gen Pract. 2018 Apr;47(4):212-215.
- 2. Scrivani SJ, Keith DA, Kaban LB. Temporomandibular disorders. N Engl J Med.2008 Dec 18;359(25):2693-705.PubMed.
- 3. Buescher JJ Temporomandibular joint disorders. Am Fam Physician. 2007 Nov 15;76(10):1477-82.PubMed
- 4. Bordoni B, Varacallo M. Stat Pearls[Internet. Stat Pearls Publishing; Treasure Island (FL):Jul17, 2023. Anatomy, Head and Neck, Temporomandibular Joint. PMC free article [PubMed.
- 5. Kucukguven, A.; Demiryurek, M.D.; Vargel, I. Temporomandibular joint innervation:Anatomical study and clinical implications. Ann. Anat. 2022, 240, 151882.
- 6. Ingawalé, S.; Goswami, T. Temporomandibular joint: Disorders, treatments, and biomechanics. Ann. Biomed. Eng. 2009, 37, 976–996.
- 7. Solberg WK. Temporomandibular joint syndrome. Semin Neurol.1988 Dec;8(4):291-7. PubMed.
- 8. Scrivani SJ, Keith DA, Kaban LB. Temporomandibular disorders. NEnglJMed. 2008 Dec18;359 (25):2693-705.PubMed
- 9. Young AL. Internal derangements of the temporomandibular joint:A review of the anatomy, diagnosis, and management. J Indian Prosthodont Soc. 2015 Jan-Mar;15(1):2-7.
- 10. Oral, K.; BalKüçük,B.; Ebeo-lu,B.; Dinçer, S. Etiology of temporomandibular disorder pain. AGRI 2009,21,89–94.
- 11. Sharma S, Gupta DS, Pal US, Jurel SK. Etiological factors of temporomandibular joint disorders. Natl J Maxillofac Surg. 2011 Jul;2(2):116-9.PMC free article [PubMed]
- 12. Liu F, Steinkeler A. Epidemiology, diagnosis,and treatment of temporomandibular disorders. Dent Clin North Am. 2013 Jul;57(3):465-79.
- 13. Cooper BC, Kleinberg I. Examination of a large patient population for the presence of symptoms and signs of temporomandibular disorders. Cranio. 2007 Apr;25(2):114-26.
- 14. Pasinato, F.; Souza, J.A.; Corrêa, E.C.R.; Silva,A.M.T.Temporomandibular disorder and generalized joint hypermobility: Application of diagnostic criteria. Braz. J. Otorhinolaryngol. 2011, 77, 418–425.
- 15. Peck,C.C.; Goulet, J.P.; Lobbezoo, F.; Schiffman, E.F.; Alstergren, P.; Anderson, G.C.; DeLeeuw, R.; Jensen, R.; Michelotti, A.; Ohrbach, R.; et al. Expanding the taxonomy of the diagnostic criteria for temporomandibular disorders. J. Oral Rehabil. 2014, 41, 2–23.
- 16. Okeson JP, deLeeuw R. Differential diagnosis of temporomandibular disorders and other orofacial pain disorders. Dent Clin North Am. 2011 Jan;55(1):105-20.PubMed.
- 17. Reneker J, Paz J, Petrosino C, Cook C. Diagnostic accuracy of clinical tests and signs of temporo mandibularjointdisorders:asystematicreviewo ftheliterature.J Orthop Sports Phys Ther. 2011 Jun;41(6):408-16.PubMed
- 18. Manfredini, D.; Guarda-Nardini, L.; Winocur, E.; Piccotti, F.; Ahlberg, J.; Lobbezoo, F. Research diagnostic criteria for temporomandibular disorders: A systematic review of axis I epidemiologic findings. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontol.2011, 112, 453–462.
- 19. Talmaceanu D, Lenghel LM, Bolog N, Hedesiu M, Buduru S, Rotar H, Baciut M, Baciut G. Imaging modalities for temporomandibular joint disorders: an update. Clujul Med. 2018 Jul;91(3):280-287.PMC free article [PubMed
- 20. Vogl TJ, Lauer HC, Lehnert T, Naguib NN,OttlP,Filmann N, Soekamto H, Nour EldinNE. The value of MRI in patients with temporomandibular joint dysfunction: Correlation of MRI and clinical findings. Eur J Ra.
- 21. Lewis EL, Dolwick MF, Abramowicz S, Reeder SL. Contemporary imaging of the temporomandibular joint. Dent Clin North Am. 2008 Oct;52(4):875-90, viii.
- 22. Schiffman, E.; Ohrbach, R. Executive summary of the Diagnostic Criteria for Temporomandibular Disorders for clinical and research applications. J. Am. Dent. Assoc. 2016, 147, 438–445.
- 23. Chellappa, D.; Thirupathy, M. Comparative efficacy of low-Level laser and TENS in the symptomatic reliefoftemporomandibularjoin tdisorders :Arandomizedclinicaltrial. IndianJ. Dent.Res.2020,31,42–47.
- 24. Urbański, P.; Trybulec, B.; Pihut, M. The Application of Manual Techniques in Masticatory Muscles Relaxation as Adjunctive Therapy in the Treatment of Temporomandibular Joint Disorders. Int. J. Environ. Res. Public Health 2021, 18, 12970.
- 25. Ziaeifar, M.; Arab, A.M.; Mosallanezhad, Z.; Nourbakhsh, M.R. Dry needling versus trigger point compression of the upper trapezius: A randomized clinical trial with two weeks & three-month follow- up. J. Man. Manip. Ther.2019, 27, 152–161.
- 26. Calixtre, L.B.; Grüninger, B.L.; Haik, M.N.; Alburquerque-Sendín, F.; Oliveira, A.B. Effects of cervical mobilization and exercise on pain, movement and function in subjects with temporomandibular disorders: A single group pre- post test. J. Appl. Oral Sci. 2016, 24, 188–197.
- 27. Madani, A.S.; Mirmortazavi, A. Comparison of three treatment options for painful temporomandibular joint clicking. J. Oral Sci. 2011, 53, 349–354.
- 28. Dib-Zakkour, J.; Flores-Fraile, J.; Montero-Martin, J.; Dib-Zakkour, S.; Dib Zaitun, I. Evaluation of the Effectiveness of Dry Needling in the Treatment of Myogenous Temporomandibular Joint Disorders.
- 29. Gauer, R.L.; Semidey, M.J. Diagnosis and treatment of temporomandibular disorders. Am.Fam. Physician 2015, 91, 378–386.
- 30. Wieckiewicz, M.; Boening, K.; Wiland, P.; Shiau, Y.Y.; Paradowska-Stolarz, A. Reported concepts for the treatment modalities and pain management of temporomandibular disorders. J. Headache Pain 2015, 16, 106.
Data Sharing Statement
Funding
Author Contributions
Ethics Declaration
Acknowledgements
Conflicts of Interest
About this article
Cite this article
Misra A, Pal A, Jain P, et al. Effect of physiotherapy intervention in temporomandibular joint dysfunction. Physio Ther Occup Ther J. 2024;17(3):133-139.
Licence:
Attribution-Non-commercial 4.0 International (CC BY-NC 4.0)This license enables reusers to distribute, remix, adapt, and build upon the material in any medium or format for noncommercial purposes only, and only so long as attribution is given to the creator.
| Received | Accepted | Published |
|---|---|---|
| July 09, 2024 | August 16, 2024 | September 30, 2024 |
DOI: http://dx.doi.org/10.21088/potj.0974.5777.17324.1
Keywords
Temporomandibular joint dysfunctionphysiotherapypain managementmuscle tensionconservative treatmentmanual therapydry needlingrehabilitationcase reportTMJ disorders.physiotherapypain managementmuscle tensionconservative treatmentmanual therapydry needlingrehabilitationcase reportTMJ disorders.Search for Similar Articles
Similar Articles
- Exploring the Connection Between Stress, Anxiety, and Central Pain Mechanisms
- Comparative Effectiveness of Mulligan SNAGs and the McKenzie Method in the Mana...
- To Compare the Effectiveness of Dual Task Training Versus Task Oriented Circuit...
- Role of Virtual Reality in Physiotherapy
- Normative Values of One Leg Stance in Urban Adults of 20-40 Years
Article Level Metrics
Last UpdatedSaturday 07 February 2026, 20:24:16 (IST)
Accesses
Citations
Download citation
Article Keywords
Keyword Highlighting
Highlight selected keywords in the article text.
Timeline
| Received | July 09, 2024 |
| Accepted | August 16, 2024 |
| Published | September 30, 2024 |
licence
This license enables reusers to distribute, remix, adapt, and build upon the material in any medium or format for noncommercial purposes only, and only so long as attribution is given to the creator.