Original Article
Hyperpara Thyroidism and its Management
Licence:
Attribution-Non-commercial 4.0 International (CC BY-NC 4.0)This license enables reusers to distribute, remix, adapt, and build upon the material in any medium or format for noncommercial purposes only, and only so long as attribution is given to the creator
RFP Journal of ENT and Allied Sciences 8(1):p 9-12, January-June 2023. | DOI: N/A
How Cite This Article:
Kaur S, Subashini SP, Jain P. Hyperparathyroidism and its management. RFP J ENT Allied Sci. 2023;8(1):9–12.Timeline
Abstract
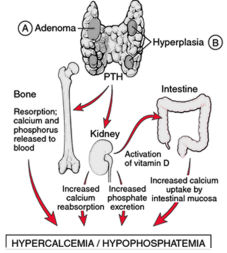
Hyperparathyroidism is an increase in parathyroid hormone (PTH) levels in the blood. This occurs from a disorder either within the parathyroid glands (primary hyperparathyroidism) or as response to external stimuli (secondary hyperparathyroidism). Symptoms of hyperparathyroidism are caused by inappropriately normal or elevated blood calcium leaving the bones and flowing into the blood stream in response to increased production of parathyroid hormone. In healthy people, when blood calcium levels are high, parathyroid hormone levels should be low. With long-standing hyperparathyroidism, the most common symptom is kidney stones. Other symptoms may include bone pain, weakness, depression, confusion, and increased urination. Both primary and secondary may result in osteoporosis (weakening of the bones). In 80% of cases, primary hyperparathyroidism is due to a single benign tumor known as a parathyroid adenoma. Most of the remainder are due to several of these adenomas. Very rarely it may be due to parathyroid cancer. Secondary hyperparathyroidism typically occurs due to vitamin D deficiency, chronic kidney disease, or other causes of low blood calcium. The diagnosis of primary hyperparathyroidism is made by finding elevated calcium and PTH in the blood.
References
- 1. https://rspmanguharjo.jatimprov.go.id /wpcontent /uploads /2020/02/11.-Handbook-for - Brunner - and - Suddarths - Textbook - of - Medical - Surgical - Nursing - 12th - Edition - Suzann.pdf
- 2. h t t p s : / / w w w . h y p e r p a r a t h y r o i d m d . c o m / hyperparathyroidism/
- 3. https://en.wikipedia.org/wiki/Hyperparathy roidism
- 4. https://www.endocrineweb.com / conditions / hyperparathyroidism / hyperparathyroidism
Data Sharing Statement
Funding
Author Contributions
Ethics Declaration
Acknowledgements
Conflicts of Interest
About this article
Cite this article
Kaur S, Subashini SP, Jain P. Hyperparathyroidism and its management. RFP J ENT Allied Sci. 2023;8(1):9–12.
Licence:
Attribution-Non-commercial 4.0 International (CC BY-NC 4.0)This license enables reusers to distribute, remix, adapt, and build upon the material in any medium or format for noncommercial purposes only, and only so long as attribution is given to the creator
| Received | Accepted | Published |
|---|---|---|
| April 24, 2023 | May 25, 2023 | June 30, 2023 |
DOI: N/A
Keywords
Vitamin DOsteoporosisParathoromoneRenal RicketsSearch for Similar Articles
Similar Articles
- Pseudomonas Aeruginosa in an Immunocompetent Individual with Acute Tonsillitis;...
- Hidden Dangers of Oral Hygiene: Oropharyngeal Impalement by Toothbrush in a 3-Ye...
- Functional Outcome of Abbe–Estlander Flap in Lower Lip Carcinoma with Commissura...
- Primary Laryngeal Histoplasmosis
- Inverted Papilloma a Retrospective Study of 17 Cases
Article Level Metrics
Last UpdatedMonday 26 January 2026, 18:54:45 (IST)
Accesses
Citations
Download citation
Article Keywords
Keyword Highlighting
Highlight selected keywords in the article text.
Timeline
| Received | April 24, 2023 |
| Accepted | May 25, 2023 |
| Published | June 30, 2023 |
licence
This license enables reusers to distribute, remix, adapt, and build upon the material in any medium or format for noncommercial purposes only, and only so long as attribution is given to the creator