Review Article
Antimicrobial Resistance in Paediatrics: An Alarming View
Rajathi sakthivel,, Madhumitha , D.K. Sriram
Licence:
Attribution-Non-commercial 4.0 International (CC BY-NC 4.0)This license enables reusers to distribute, remix, adapt, and build upon the material in any medium or format for noncommercial purposes only, and only so long as attribution is given to the creator.
Journal of Emergency and Trauma Nursing 5(2):p 53-59, July - Dec 2024. | DOI: n.a
How Cite This Article:
Madhumitha, Rajathisakthivel, Sriram DK. Antimicrobial Resistance in Paediatrics: An Alarming View. J Emerg Trauma Nurs. 2024;5(2):53-59.Timeline
Abstract
A major global problem is antimicrobial resistance (AMR), particularly in pediatrics because of the immature immune systems. Multidrug-resistant organisms (MDROs) are a result of the overutilization and abuse of antibiotics as well as a dearth of data specifically about children, leading to severe and prolonged illness, longer hospitalization times, and higher mortality rates. The root causes include Improper use of antibiotics, lack of pediatricspecific data, and specific contraindications for certain antibiotics. Genetic and evolutionary factors also contribute to antibiotic resistance, with mutations allowing resistant strains to evolve and survive. Resolving these problems is essential to halting the rise of germs resistant to antibiotics and enhancing public health. Overcoming AMR in pediatrics involves optimizing antibiotic use, promoting antimicrobial stewardship programs, implementing preventive measures like vaccination, and integrating infection prevention and control practices. Governments and international organizations must lead to fight against antibiotic resistance by developing policies that encourage appropriate antibiotic use, support public health initiatives, fund research and development of new antibiotics, and implement stringent regulatory measures.
References
- 1. Pana, Z.D., El-Shabrawi, M., Sultan, M.A., Murray, T., (2023). Fighting the hidden pandemic of antimicrobial resistance in paediatrics: recommendations from the International Pediatric Association. BMJ paediatrics open, 7(1), e002084. https://doi.org/10.1136/bmjpo-2023-002084 . https://doi.org/10.1136/bmjpo-2023-002084 . https://doi.org/10.1136/bmjpo-2023-002084.
- 2. Yu, D., Zheng, Y., Shen, A., Wu, F., Dmitriev, A. V., Kilian, M., & Yang, Y. (2023). Editorial: Antimicrobial resistance in pediatric infectious diseases: antimicrobial resistance, resistance mechanisms and antimicrobial use. Frontiers in Cellular and Infection Microbiology, 13. https:// doi.org/10.3389/fcimb.2023.1287051.
- 3. Logan, L.K., Braykov, N.P., Weinstein, R.A., & Laxminarayan, R. (2014). Extended-Spectrum B-Lactamase–Producing and Third-Generation Cephalosporin-Resistant Enterobacteriaceae in Children: Trends in the United States, 1999– 2011. Journal of the Pediatric Infectious Diseases Society, 3(4), 320–328. https://doi.org/10.1093/ jpids/piu010
- 4. Gandra, S., Tseng, K.K., Arora, A., Bhowmik, B., Robinson, M.L., Panigrahi, B., Laxminarayan, R., & Klein, E. Y. (2019). The Mortality Burden of Multidrug-resistant Pathogens in India: A Retrospective, Observational Study. Clinical infectious diseases : an official publication of the Infectious Diseases Society of America, 69(4), 563–570. https://doi.org/10.1093/cid/ciy955
- 5. Gussin GM, McKinnell J.A., Singh R.D., et al. Reducing Hospitalizations and MultidrugResistant Organisms via Regional Decolonization in Hospitals and Nursing Homes. JAMA. 2024; 331(18):1544–1557. doi:10.1001/jama.2024.2759.
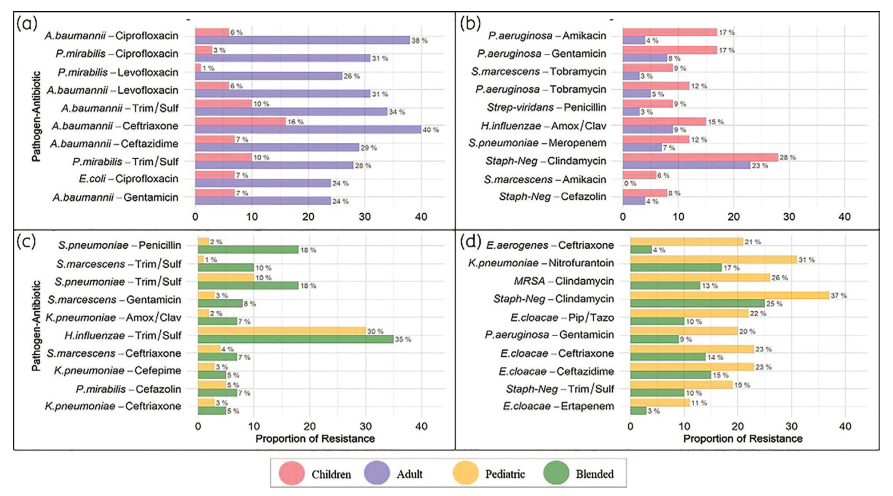
- 6. Sivasankar, S., Goldman, J.L., & Hoffman, M.A. (2022). Variation in antibiotic resistance patterns for children and adults treated at 166 non-affiliated US facilities using EHR data. JAC-Antimicrobial Resistance, 5(1). https://doi. org/10.1093/jacamr/dlac128
- 7. Eva Degraeuwe, Pirkko Lepola, Mark Turner, Kim Jennings, Lieve Nuytinck, Ann Raes, Karel Allegaert, Johan Vande Walle, Fenna Mahler - 31 An update on the challenges of conducting pediatric clinical trials: 15 years of progress since EMA regulation implementation: BMJ Paediatrics Open 2024;
- 8. Romandini, A., Pani, A., Schenardi, P.A., Pattarino, G.A.C., De Giacomo, C., & Scaglione, F. (2021). Antibiotic Resistance in Pediatric Infections: Global Emerging Threats, Predicting the Near Future. Antibiotics, 10(4), 393. https:// doi.org/10.3390/antibiotics10040393
- 9. Årdal, C., Balasegaram, M., Laxminarayan, R., McAdams, D., Outterson, K., Rex, J.H., &
- 10. Ahmed, S.K., Hussein, S., Qurbani, K., Ibrahim, R.H., Fareeq, A., Mahmood, K.A., & Mohamed, M.G. (2024). Antimicrobial resistance: Impacts, challenges, and future prospects. Journal of Medicine Surgery and Public Health, 2, 100081. https://doi.org/10.1016/j.glmedi.2024.100081
- 11. Ho, C.S., Wong, C.T.H., Aung, T.T., Lakshminarayanan, R., Mehta, J.S., Rauz, S., McNally, A., Kintses, B., Peacock, S.J., De La Fuente-Nunez, C., Hancock, R.E.W., & Ting, D.S.J. (2024). Antimicrobial resistance: a concise update. The Lancet Microbe, 100947. https://doi. org/10.1016/j.lanmic.2024.07.010
- 12. Jacobs, M.R., & Dagan, R. (2004). Antimicrobial resistance among pediatric respiratory tract infections: clinical challenges. Seminars in Pediatric Infectious Diseases, 15(1), 5–20. https:// doi.org/10.1053/j.spid.2004.01.003
- 13. Wang, J., He, L., Sha, J., Zhu, H., Huang, L., Zhu, X., Dong, J., Li, G., Ge, Z., Lu, R., Ma, G., Shi, Y., & Guo, Y. (2018). Etiology and antimicrobial resistance patterns in pediatric urinary tract infection. Pediatrics International, 60(5), 418–422.
- 14. Mohamed, A.A., Bastug, Y., Senol, C., Kassim, M.M., Yusuf, A.A., & Mohamed, A.H. (2020). Antimicrobial resistance pattern and uropathogens distribution in children visiting a referral hospital in Mogadishu. Future Science OA, 10(1). https:// doi.org/10.2144/fsoa-2023-0298
- 15. The urgent threat of drug-resistant infections protecting children worldwide a unicef guidance note on antimicrobial resistance - https:// www.unicef.org/media/144266/file/TheUrgent-Threat-of-Drug-Resistant-Infections:- A-UNICEF-Guidance-Note-on-AntimicrobialResistance-2023.pdf
- 16. Threats of Antimicrobial Resistance (AMR) in Pediatrics, July 3, 2022, Posted in: AMR Writers Participants’ Articles, Articles, Educational Resources, By Jimmy Nkaiwuatei& Janice Odhiambo, https://www. studentsagainstsuperbugs.org/educationalresources/threats-of-antimicrobial-resistanceamr-in-pediatrics/ accessed on 16 November 2024
- 17. Abo, Y., Freyne, B., Kululanga, D., & Bryant, P. A. (2022). The Impact of Antimicrobial Stewardship in Children in Low- and Middleincome Countries. The Pediatric Infectious Disease Journal, 41(3S), S10–S17. https://doi. org/10.1097/inf.0000000000003317
- 18. Shrestha, J., Zahra, F., & Cannady, P., Jr. (2023, June 20). Antimicrobial Stewardship. StatPearls - NCBI Bookshelf. https://www.ncbi.nlm.nih. gov/books/NBK572068/
- 19. Rezk, A.R., Bawady, S.A., & Omar, N.N. (2021). Incidence of emerging multidrug-resistant organisms and its impact on the outcome in the pediatric intensive care. Egyptian Pediatric Association Gazette, 69(1). https://doi. org/10.1186/s43054-021-00071-1
- 20. Banerjee, R., & Patel, R. (2022). Molecular diagnostics for genotypic detection of antibiotic resistance: current landscape and future directions. JAC-Antimicrobial Resistance, 5(1). https://doi.org/10.1093/jacamr/dlad018
- 21. Antimicrobial Resistance: Tackling a crisis for the health and wealth of nations,The Review on Antimicrobial Resistance Chaired by Jim O’Neill December 2014.
- 22. Storr, J., Twyman, A., Zingg, W., Damani, N., Kilpatrick, C., Reilly, J., Price, L., Egger, M., Grayson, M.L., Kelley, E., & Allegranzi, B. (2017). Core components for effective infection prevention and control programmes: new WHO evidence-based recommendations. Antimicrobial Resistance and Infection Control, 6(1). https:// doi.org/10.1186/s13756-016-0149-9.
- 23. Union for International Cancer Control (UICC) , Antimicrobial resistance and its impact on cancer care, 21 November 2023 https://www.uicc. org/what-we-do/thematic- reas/antimicrobialresistance-amr?gad_source=1&gclid=Cj0KCQiA ire5BhCNARIsAM53K1hp2w4pUIN1knwa7fcrb
Data Sharing Statement
Funding
Author Contributions
Ethics Declaration
Acknowledgements
Conflicts of Interest
About this article
Cite this article
Madhumitha, Rajathisakthivel, Sriram DK. Antimicrobial Resistance in Paediatrics: An Alarming View. J Emerg Trauma Nurs. 2024;5(2):53-59.
Licence:
Attribution-Non-commercial 4.0 International (CC BY-NC 4.0)This license enables reusers to distribute, remix, adapt, and build upon the material in any medium or format for noncommercial purposes only, and only so long as attribution is given to the creator.
| Received | Accepted | Published |
|---|---|---|
| November 26, 2024 | December 28, 2024 | December 31, 2024 |
DOI: n.a
Keywords
Antimicrobial resistanceAntibioticsMultidrug-resistant organismAntimicrobial stewardship programs and preventive measuresSearch for Similar Articles
Similar Articles
- Recent Advances in Surgical Nursing
- Trauma Nursing Management: A Comprehensive Approach to Patient Care in Acute and...
- Planned Teaching Strategy on Knowledge Regarding Prevention of Home and Miscella...
- A Study to assess the Knowledge Regarding Tracheostomy Care among Critical Care...
- Oxygen Administration and the Vital Role of Nurses: A Comprehensive Review
Article Level Metrics
Last UpdatedSaturday 07 February 2026, 10:25:11 (IST)
Accesses
Citations
Download citation
Article Keywords
Keyword Highlighting
Highlight selected keywords in the article text.
Timeline
| Received | November 26, 2024 |
| Accepted | December 28, 2024 |
| Published | December 31, 2024 |
licence
This license enables reusers to distribute, remix, adapt, and build upon the material in any medium or format for noncommercial purposes only, and only so long as attribution is given to the creator.